A Real Pain in the A**! Coccyx Pain 101
- Nomadic Physical Therapy PLLC
- Feb 1, 2024
- 8 min read
Serving as the medical term for tailbone, the coccyx is a very important, yet delicate bony structure at the base of the human spine. When there is pain in the coccyx region, it is called coccygodynia.
Solving coccyx pain is similar to soothing a crying baby…sometimes it’s as straightforward as giving the baby a bottle. But sometimes it can require a complex combination of variables to finally calm things down. Reducing coccyx pain can require more persistence than some other pelvic issues, of which typically leads to multiple medical providers, various trialed treatments, and for some unfortunate individuals, years of chronic pain before finally finding relief.
But WE CAN CHANGE THAT NARRATIVE! And it starts right here, with education on what coccygodynia is and what your options are if you experience it.

First let’s take a look at the anatomy of the structure. The coccyx makes up the last 3-5 segments of your spine. It's nickname, the tailbone, is very fitting as the coccyx can move forward, like a dog tucking its tail between its legs. But it also has the ability to extend backward, opening up the pelvic outlet. There is great variability in the size and fixation of the coccyx in each individual. In fact, these segments are even fused together in about 10% of individuals.
Though fairly small in size, this group of bones is well supported by 6 thick ligaments that attach and secure it to the pelvis. Additionally, 5 muscles groups attach and support the function of the coccyx, composing the following list of direct soft tissue connections:
Pubococcygeus *
Iliococcygeus *
External anal sphincter *
Coccygeus *
Posterior/anterior coccygeal ligaments
Sacrococcygeal ligament
Sacrospinous ligament
Sacrotuberous ligament
Gluteus maximus muscles
* part of the pelvic floor muscle group

Because of these various soft tissue connections, the coccyx has a limited range of movement of 22 degrees total. Like the other regions of the spine, the coccyx can flex, extend, and laterally bend. Interestingly, coccyx movement matches that of the lumbar spine…so if I side bend to the right, my coccyx will also deviate to the right. If I bend backwards, my coccyx will extend…you get the idea. Additionally, the muscles can influence the resting position of the coccyx. For example, extension occurs when the pelvic floor muscles relax, such as during defecation and birthing (Grassi et al., 2007) versus, if the pelvic floor contracts, such as during a kegel, the coccyx will tuck under.

So What Causes the Pain?
When differentiating between what might be contributing to coccyx pain, there are many aspects to consider. With a thorough assessment, a medical provider should be considering the following possibilities:
A bone fracture from a past injury? Such as a fall or traumatic birth?
Pelvic floor tension?
Gluteal tension referral?
Is the sacrococcygeal joint too stiff / hypomobile?
Is the sacrococcygeal joint lacking stability? History of dislocation, hypermobility, or dynamic instability?
Presence of a bone spur
Arthritis of the sacrococcygeal joint
Neural tension/nervous system pain
Presence of a Cyst? Such as a Tarlov cyst *
Osteomyelitis *
Cancer?* Tumor?*
* Indicating a red flag with immediate referral to a medical provider that can utilize imaging and other diagnostic tests to rule out.
Who Typically Reports Tailbone Pain?
Due to its location at the base of the pelvis, it is typically individuals who place increased pressure on the structure that experience coccyx pain, particularly for long durations, such as cyclists, rowers, horseback riders.
In my clinical experience, I’ve treated clients with coccygodynia from prolonged sitting at their desk for work and those who frequently travel for work. There was a large influx of clients reporting pain when transitioning from the workplace to working remotely from home, of which I contribute to poor ergonomic set up of their workstations, with many individuals admitting they were working from a semi-reclined position in their bed, from their couch, or kitchen table.
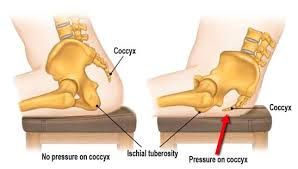
Coccyx pain from childbirth is not uncommon since the baby has to make his/her way through the pelvic outlet…if the mother’s tailbone does not have enough space to extend (opening up the pelvic outlet) such as say lying on her back with her tailbone pressing into the bed, increased stress on the coccyx may occur. Coccyx fractures from childbirth are far less common, but there is a risk with increased size of baby or need for vacuum or forceps assistance during delivery.
Anyone who has experienced a fall onto their tailbone can describe exactly how uncomfortable landing on the tailbone can be. Whether slipping on ice, losing balance on your roller blades, or getting pushed down in a sport…the tailbone does not absorb impact well. And the body seems to ‘remember’ these injuries…I’ve treated clients who continue to experience their coccyx pain in adulthood from a fall they had as a child or teenager. Oftentimes, the human nervous system stays on “high guard” to protect from further injury, but this can contribute to increased muscular tension and actually accentuate pain levels.
Coccyx pain is also commonly seen in individuals that have had a pelvic surgery, of really any kind. Cesarean section, abdominal laparoscopy, cyst removal, lumbar fusion/discectomy, labral repair, hysterectomy, bladder mesh, prolapse repair, hemorrhoidectomy, anal fissure repair, etc. This is due to that vast network of soft tissues that connect onto the coccyx directly, plus all of the fascial connections contributing to the posterior chain and core complex of the trunk. It’s all connected!
Now what’s interesting is that research states that coccygodynia occurs 5x more often in women than men (Lirette, Chaiban & Eissa, 2014). In my personal experience, I’ve treated more men with coccygodynia than women, particularly police officers and construction workers who have had to wear a weighted belt for hours on end. This affected the posture of their spine when standing and greatly contributed to their coccyx pain. I’ve typically seen women experience most of their coccyx pain during pregnancy and the post-partum phase. But this could continue to change over time.
I Have Tailbone Pain…What Should I Do About It?
Here’s the good news…there are so many options of interventions to try in addressing your coccyx pain and the majority of them are conservative options!
The most straightforward and cheapest options are icing or taping the region (Youtube kinesiotaping for tailbone pain and numerous videos will pop up).
Cushions can be life changing for some, particularly if you have to sit for prolonged periods of time. However, you might have to try out a few types before you find a good fit. Instead of a donut cushion (which would actually put pressure directly onto the tailbone, think about a cushion with a cutout - see picture below). Think about one for your car, desk chair or any other chair you would sit in for a prolonged period of time. Don’t forget to pack it with you for flights!
A couple recommendations are Cushion Your Assets, www.theraseat.com

Now if you google “tailbone pain relief”, the next suggestion is going to be topical or oral medications such as non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen, opioids, baclofen. Personally and professionally, I believe there are appropriate times to utilize these types of medications, but know that while they may help reduce the pain temporarily, medications will not solve the root cause of your tailbone pain.
The interventions that I have found to be most effective for many: activity modification, ergonomic adjustments, and physical therapy. A physical therapist can take a holistic approach in helping understand any and all contributors to your tailbone pain. A thorough assessment can reveal muscular imbalances, joint limitations, neural tension contributors to your pain. A pelvic floor physical therapist can provide manual interventions (via massage, stretching, mobilization and manipulation. This can include internal and/or external contact with the coccyx), education on activity modification and ergonomic adjustments to address the root cause of your tailbone pain.
If the above conservative options have not helped as expected, there are still additional options, of which would need to be discussed with your medical doctor. These include:
Steroid injections
Ganglion impar blocks
Nerve ablation
Coccygectomy (surgical removal of the coccyx)
I deeply encourage you to seek out various opinions and take great consideration of your goals/lifestyle and expectations before considering these options as I have seen too many clients undergo these procedures having spent hundreds of dollars with minimal change to their pain. Additionally, there are greater risks to these types of procedures such as risk of wound infection, bone infection, persistent chronic pain, and pelvic organ prolapse.
While I am biased that conservative treatment, particularly pelvic floor physical therapy, would be beneficial for anyone experiencing coccygodynia to try…it is for a validated reason. In a 2014 study, conservative treatment (ie: pelvic floor therapy) was shown to be 90% successful in resolving pain of the coccyx! (Lirette et al 2014). Another study in 2017 noted 72% improvement of pain when chronic coccydynia was addressed with pelvic floor physical therapy (Scott et al 2017). So whether you’ve just noticed your pain or you’ve dealt with pain for years, your chance of experiencing improvements with pelvic floor physical therapy is fairly high!
What To Expect from Pelvic Floor Physical Therapy?
Trying something new can be scary, particularly when it has to do with the pelvic region. At your first appointment, your pelvic floor therapist will ask you some questions like:
How long have you had your pain?
Have you had any specific injuries to your tailbone? Have you ever injured your foot or leg? Have you had any surgeries?
Does your pain change if you're sitting vs when you’re standing/walking?
Do you get pain during the transition from sitting to standing?
Does the type of surface you sit on make a difference? Soft vs firm?
Do you have any pain while sitting on the toilet? How about during/after a bowel movement?
Do you have any pain during intercourse?
These questions provide valuable insight of what structure and movements might be contributing to your pain. Even a past ankle sprain can affect how you stand/walk and contribute to the position of your pelvis, so your therapist should be very thorough when asking you these questions. Additionally, they should ask you what your goals are for addressing your pain…Do you want to be able to cycle again? Do you have an upcoming flight overseas and need to be able to sit for travel? Maybe you want to be able to make it through a yoga class without limitations?
If you’re comfortable proceeding with the evaluation, the therapist will then assess how you move. They may ask to see you squat, bend forward and backward. They may ask to place a hand on your tailbone as you perform these movements to track how the coccyx is moving as you move your lumbar spine. Additionally, they may assess your hip mobility and strength, see if you have any tension in your hip and back muscles. If deemed necessary, they may ask you if you’re comfortable having your pelvic floor muscles evaluated- again due to the connections of the pelvic floor muscles onto the coccyx bone.
These observations will help the physical therapist design an individualized treatment plan to reduce your pain and help you reach your goals. With a thorough assessment, individualized treatment interventions, and consistency with the providers recommendations for activity modifications or exercises, you should notice improvements within 6 weeks. Some will experience complete relief within 12 weeks, whereas those with chronic pain may require ~6 months for pain to resolve.
If coccyx pain is something affecting you, please know there are numerous options available to address it. Here at Nomadic Physical Therapy, Dr. Mariah Lohr is specialized in treatment of pelvic floor issues such as coccygodynia.
Contact her at nomadicphysicaltherapy@gmail.com for more information.

.png)



Comments